Tenacious ME
Tackling disabling autoimmune disease with obstinance and humor.
Best Gifts for Rheumatoid Arthritis 2020 Edition

This post contains affiliate links. If you use them, I may get a commission. Thank you!
If you have a loved one with Rheumatoid Arthritis (RA), you have probably noticed that it comes with its own set of challenges. Aching joints, exhaustion, and physical limitations are likely to rule their lives. Give them the gift of relief this year! We polled 100’s of RA patients to find out what they wish for. Here’s what they asked for! From gifts to keep them warm and toasty to gadgets that will help them get things done, our readers had a ton of great ideas! Read on to find out what your arthritic loved one would be overjoyed to unwrap this year!
Topping the wishlist this year, and hitting this writer right in the feels, the number one requested gift in 2020, by a landslide, is time with the ones they love! The prolonged isolation from grandchildren, adult children, parents, friends, and all of their people has taken a toll. Holiday traditions have taken a hard hit. The result? What they’d like most of all is the magical gift of your presence.
Since the….let’s just call it 2020 chaos, shows no sign of slowing before year’s end, and many RA patients take immune suppressing medications that leave them vulnerable to that which shall not be named (look I am willing to try anything to weaken it’s power at this point), they understand that an in person visit might not be possible. That said, it’s still at the top of the list, so consider how you can be there (safely) for them.
Consider planning a visit if at all possible. The love you share and the memories you make will be well worth the time and effort it takes to make that happen, even if you have to spend 2 weeks hunkered down at home first to be sure you’re not contagious. If that’s not possible, consider ways you can visit from a distance; video call, write letters, have food delivered and have dinner “together” online, plan a virtual family game night. You may have to get creative to create the “togetherness” they are yearning for.
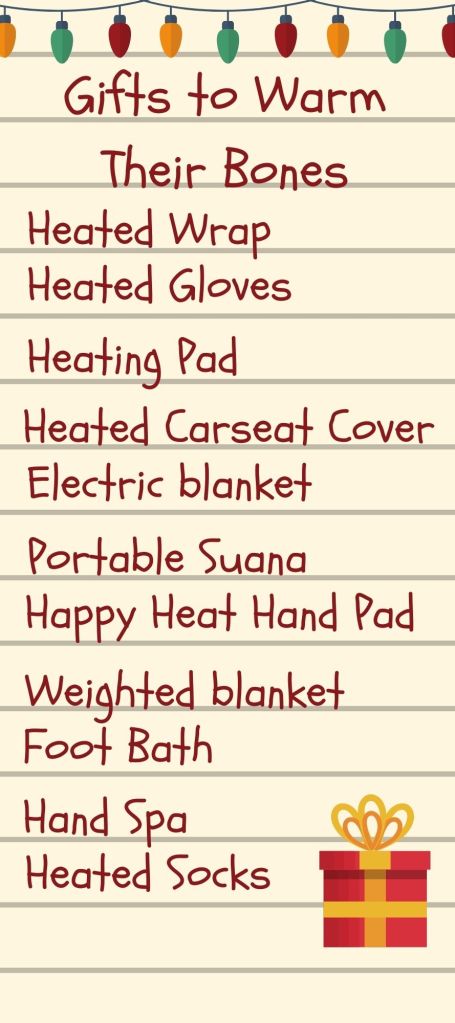
If you can’t be there, because realistically that is going to be the case for a great many people, consider sending your loved one the gift of warmth. While not quite as lovely as a hug, rheumatoid patients agreed the thing they wanted most was a heated wrap, bonus points if it is portable!
Beautyrest Ultra Soft Sherpa Berber Fleece Electric Poncho Wrap Blanket Heated Throw with Auto Shutoff, 50″ W x 64″ L, Tan PlaidKnowing that nothing ticks arthritis off more than getting “chilled to the bone” in chilly winter weather, there were many other wonderful gifts on their wishlist to keep them warm, including these cozy heated gloves, heated socks, or a nice heated carseat cover.
To help soothe chilled bones at home they asked for electric blankets and heating pads, or how about this amazing portable sauna? (Yes please!) Basically, if it makes heat to make you warm and cozy, it’s a great gift for all of the arthritis sufferers on your list.

Considering their obvious love of all things warm and cozy, it is not at all surprising that the next most frequently asked for gifts included a pile of warm and cozy socks and slippers. Leaning into the 2020 lougewear trend, leggings and pj’s were also at the top of their list.
For those increasingly rare times they need to leave the house, RA patients asked for warm gloves and mittens and comfortable shoes like these Clarks CloudSteppers, hands down my personal favorite shoe, I like them so much I have them in three different colors.
If your loved one struggles with bulky winter coats, consider a nice warm poncho, for ease of wear. It is essentially like wearing a blanket, and as we already know, they LOVE blankets!
Speaking of things they love to wear, consider picking them up some compression gloves, knee sleeves, or other compression gear. Whatever body part they have that could use a little extra love and support, there is probably compression wear for that.
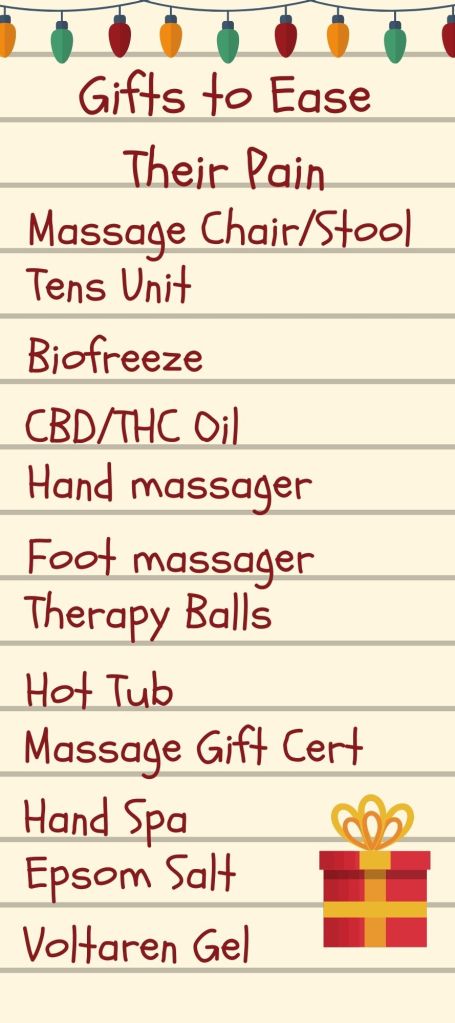
Chronic pain being one of the primary symptoms of rheumatoid arthritis, anything that will offer them a bit of relief would be greatly appreciated. The remedies that RA patients swear by include many mentholated creams, like Biofreeze. The most frequently asked for topical remedies were CBD oils and creams. Other great gift options for pain relief included bath soaks like this delightful mango soak from Scentsy or Dr Teal’s epsom salts.
To chase away the pain, those surveyed also asked for hand and foot massagers, massaging chairs, and therapy balls. Want to really make their day? A gift certificate for a massage is sure to bring them comfort and let them know you want them to feel their best.
Looking to really wow them? The dream gift among those surveyed was a hot tub! Hot tub a little out of your budget? How about a nice hand spa or foot bath instead?


Life with RA often involves a good deal of struggle with getting the little things done. Pain, inflammation, and changes in joint structure can make the simplest things a big challenge. Gadgets that can help to make those things easier will be greatly appreciated.
At the top of that wishlist were electric can openers and jar openers. I love this jar opener so much I bought a second one to keep at my Mom’s so I don’t need to ask for help there either. Other great kitchen gadgets include electric pepper mills, a Kitchen Aid stand mixer, and this amazing Rotato peeler!

For help outside of the kitchen, a lifting seat or recliner would be a great gift for your loved one who finds getting up to be a struggle. Other wonderfully helpful tools include chunky ergonomic pens, lever doorknobs, and this cool pen mouse.

Since we started out our list talking about how isolated your vulnerable loved ones are feeling this holiday season, it seems fitting to wrap up our gift guide with a list of things to help them stay entertained at home. Topping that list were gadgets that make reading easier on the hands like the Kindle Paperwhite, this amazing bookstand, and these adorable page holders. Consider keepiong those readers entertained with a subscription for a magazine, audiobook, or book of the month club.
Other great suggestions include gifts to pamper them through the long months ahead. Perhaps they would enjoy a selection of delicious teas/coffees, there are even subscription services for that. Think about the things they enjoy, you’ll likely find someone, somewhere who offers a monthly subscription box. Not sure what they would like? How about a Spoonie Box Subscription? Loaded with goodies for chronic illness fighters, it is sure to be a big hit month after month.
While the 2020 chaos might change everything, including your traditions, this year, that doesn’t mean we cannot show our isolated loved ones how very much we appreciate and care for them. A little creativity and extra effort is sure to go a long way. May your days be merry and bright and may all your test results be negative. Happy Holidays from the TenaciousME family.
What Your Loved One With Rheumatoid Arthritis Wants You To Know

One of the most frequent troubles Rheumatoid Arthritis (RA) patients struggle with is being understood. If you don’t have RA, it is a little hard to imagine what it is like. The morning stiffness that sometimes sticks around all day. The painful swollen joints, the deep fatigue, the stress of finding treatments that work and the load of side effects that often come along with treatment, make for a complex life. A life that is often also lonely as mobility becomes a challenge. Loneliness that is even deeper when friends and loved ones do not understand what they are dealing with. We polled hundreds of rheumatoid arthritis patients to find out what they wish their loved ones understood about RA. Here are a few things your loved one with Rheumatoid Arthritis wants you to know.
It isn’t arthritis
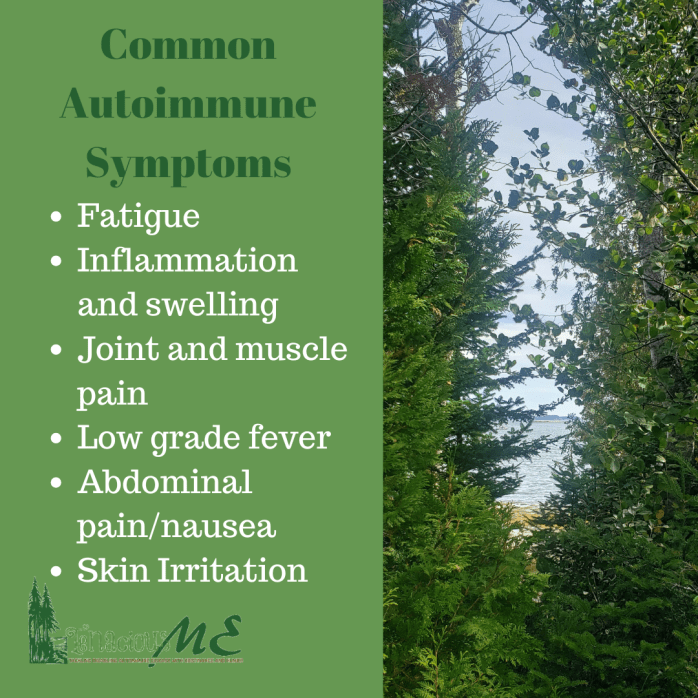
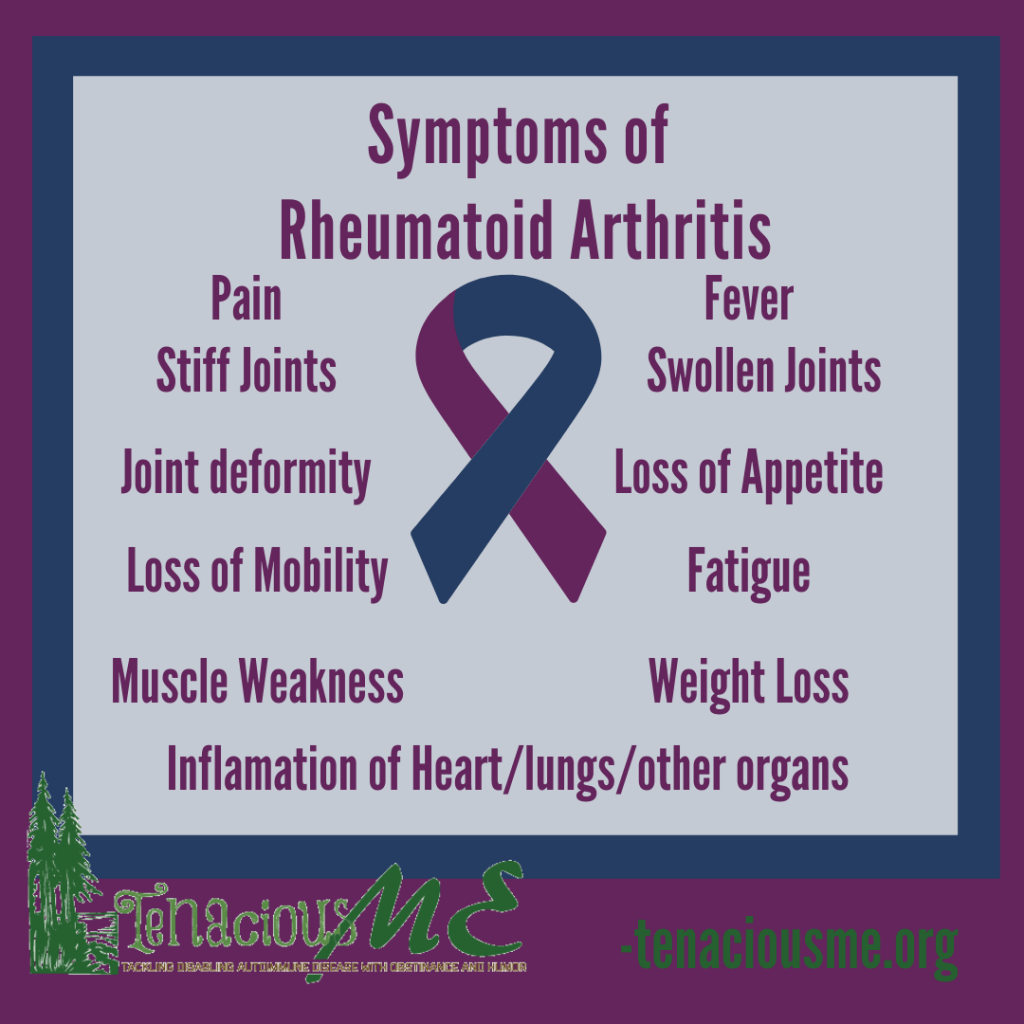
A common misconception due to the name and a general lack of knowledge about the disease, Rheumatoid Arthritis is much more than arthritis. While stiff joints, joint pain, and joint deformities are indeed a big part of how RA shows its teeth, that is far from the only area this autoimmune disease impacts.
RA is a systemic disease; this means that it attacks the entire body. Heart and lung tissue, tendons, eyes, vocal cords and muscles are also on the possible hit list for RA. It brings with it increased risk of cardiovascular disease, lung disease, various forms of cancer, wasting sickness, blindness and so much more. Unchecked, Rheumatoid Arthritis is deadly.
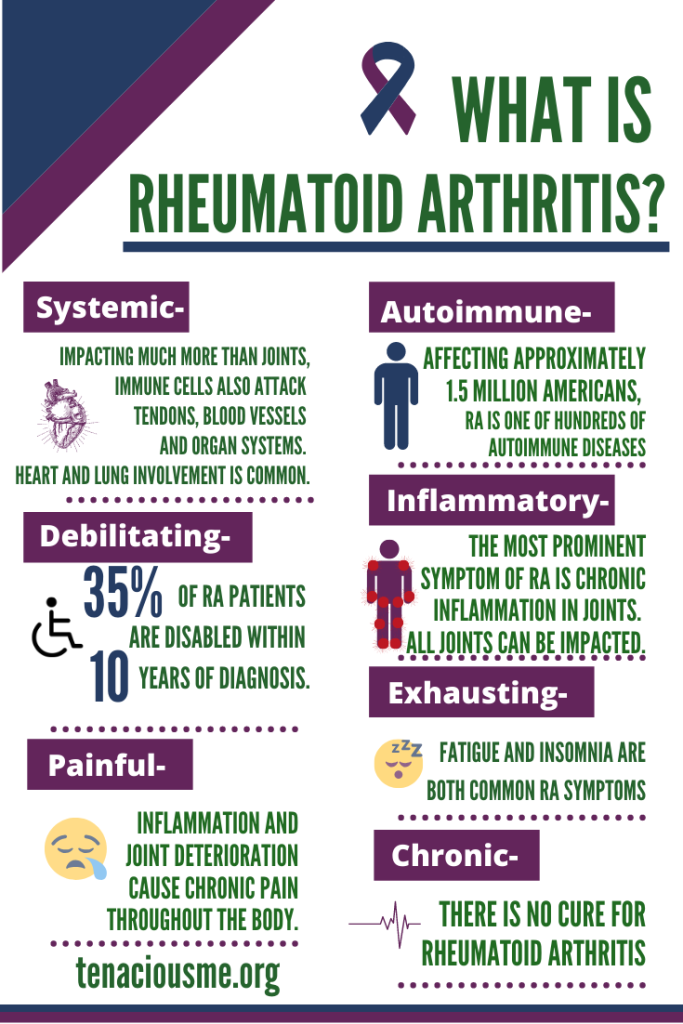
Managed, it is still chronic. The most common and persistent symptoms of disease activity are pain, stiffness, fatigue, depression, and brain fog.
Treating RA is complex, frustrating, and frightening
Fighting a chronic, debilitating disease like RA can sometimes feel like a full-time job. Medical appointments, treatments, diet and exercise regimens to keep the disease in check often dominate the lives of patients. Because even among professionals, there is a great deal of misunderstanding about the scope of the disease, patients often have to fight for the medical care they need. Successful management takes a team of professionals including rheumatologists, orthopedic doctors, physical therapists, massage therapists, psychiatrists, and various other sorts of doctors when heart, lung, eyes etc. become impacted.
Medical treatments involve medications that shut down various immune reactions, leaving patients vulnerable to a host of issues. (If your loved one with RA cringes when someone in the room sneezes, this is why!) Frequent battles with infections and microbes are par for the course.
The possible list of side effects on these medications include increased risk of cancer, nerve damage, liver failure, kidney failure, hair loss, weight gain, fatigue, blood sugar abnormalities and even destruction of bones. Treating the disease often feels as dangerous as letting it do what it will. Patients are forced to choose which side effects and symptoms they can live with, and to hope none of the ones they ignore kill them in the end.
There is no one treatment that works for all. It is all a process of trial and error. Unlike many of the symptoms humans commonly face, there is nothing that eliminates symptoms for everyone. Every body responds differently to treatment. It quickly starts to feel like a game of medical roulette, will this help, or will it destroy a vital organ? Only time and trial will tell.
There is no one treatment that works for all.
This medical mystery and frustration is doubled when faced with those who, with the best of intentions, fill them with false promises of miracle cures. The fact is,
There is no cure
Knowing all the dangers associated with active RA, you’ve likely poked around online, talked to friends, maybe even health professionals, about how your loved one could feel better and be safer. Probably more than a few have suggested diet, exercise, herbs, various medications and supplements, all with promises to cure Rheumatoid Arthritis.
Something that you really need to understand and come to terms with is THERE IS NO CURE. This disease is chronic, it is not going anywhere. While it is true that many of the recommendations will make life with Rheumatoid Arthritis and disease management easier (If you consider restrictive diets and piles of supplements easy), none of those things will ever cure RA.
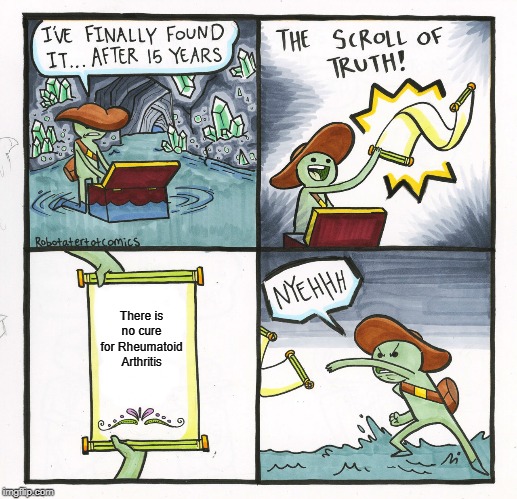
Once it is activated, there is no stopping it. The best any medical treatment or natural approach is likely to do is slow it down. In a small percentage of patients, times of “remission” may occur. Some are even able to stop medications and continue to be in remission. These cases are few and far between, and so far, none have lasted. RA always flares up eventually. Even on the most restrictive diets. Even when you do yoga daily. Even on medications with terrifying side effects.
So, while they appreciate that you want to help them feel better, please keep that miracle cure to yourself. They have heard it all before, they have probably tried it all. They are doing their best to manage their disease. What they need from you is understanding and support, leave the miracle cures to strangers on the internet. Trust me, they will get that little tidbit somewhere, and they won’t be annoyed with you for suggesting kale can cure RA.
They want to be able to do it all, they just can’t
Probably most important thing for you to know is that they are still the same person they were before RA came calling. They have the same dreams and desires, love the same activities, and truly want to live the life they lived before diagnosis. Sadly, quite often that life quickly becomes out of reach as managing RA and all the physical challenges it brings, forces them to change their lives.
They don’t have the same stamina, the pain wears them out, their bodies don’t function like they used to. Its more than pain, its debilitating muscle weakness, exhaustion, and remodeling joints. Whenever you feel annoyed that your bestie just can’t now, imagine how badly she feels about that.
Imagine you woke up tomorrow barely able to shower and dress yourself. Still think they need to just suck it up and go out with you anyway? Imagine you also woke up to find out you’d been injured by a hit and run driver in the night. That is life with Rheumatoid Arthritis.
What they can do today, they might not be able to do tomorrow (and it frustrates them more than you)
Perhaps the most challenging aspect of managing autoimmune diseases like RA is the way symptoms can change so much from one day to the next, or one end of the day to the other. Pain and inflammation flares and calms in sometimes completely unpredictable cycles. A knee that works perfectly in the morning may be stiff and useless by afternoon.
To an outsider, not living in a body that can now and truly can’t later, it is hard to imagine why rheumatoid patients cancel plans when they do. Yesterday you saw them at the gym, and they were fine, it is easy to understand why you find their claims that they can’t walk today suspect. But this is the reality of life with RA.
When they say they can’t, they mean it. Believe them and try to be sympathetic. They wanted to join you, they really did plan to enjoy that day out, but they are not in control of when they can and when they can’t. They live their lives at the mercy of unpredictable bodies.
The fact is, cancelling plans disappoints them more than it disappoints you. They do it all the time and its never because they don’t want to leave the house. They have cancelled dinners, dates, shopping plans, medical appointments, days of work, showers, projects they wanted to do. The list of times they have felt the guilt of cancelling because they woke up in a flare are endless. It makes them feel weak and useless. They never feel as though they are in control. It is unimaginably frustrating. Let them know you understand their frustration, be disappointed alongside them, not disappointed in them. They have the self-disappointment covered.
Everything is more challenging than it used to be
It is hard to imagine life with RA unless you’ve lived it. A systemic disease, it impacts every aspect of life. Unlike the more common Osteoarthritis that comes with wear and tear as we age, RA can impact even the least used joints in the body. Joints you don’t even probably realize are joints.
It does so in a very chaotic manner. There is no real rhyme or reason to what it hits and when it hits. Inflammation can pop up at any time, leaving joints swollen, hot to the touch, stiff, and painful. Anywhere in the body. From jaw hinges to the tiniest of toe joints, any body part can suddenly become useless and painful to attempt to move. This causes every aspect of life to become a challenge.
From brushing your teeth to walking out the door each day, you move a surprising number of joints. Imagine if each of them felt as though they were welded shut. If you’d like to see what that is like, take a long rope, wrap it around your dominant hand so it cannot open all the way, now, wrap it around your elbow, then secure it to your waist. Be sure not to leave enough slack to raise your arm. Now, go ahead and get washed and dressed. Did I mention that you also cannot reach your feet today? Hope you have slide on shoes and don’t mind going without socks, otherwise you better leave 30 minutes to figure out how to get those feet dressed. If you had RA, all those restrictions would also be punctuated by pain.
Since we are getting dressed, let’s take a look in that closet for a minute. Remove every item with buttons or snaps. Hands ravaged by RA, the number one symptom of the disease, cannot manage buttons and other fine motor tasks. Many an RA patient has made the mistake of struggling to button their pants only to find themselves unable to unbutton them at the crucial moment. Yes, sometimes we pee ourselves, trapped in pants we cannot undo. There is nothing much more humbling than being trapped in pee soaked pants. So, let’s just remove those from the wardrobe. Also, remove anything with a small zipper pull, also a fine motor skill, zippers are another great way to become trapped in your own clothing.

Next, let’s take a good long look at that collection of shoes. Remove anything that ties, you can’t reach the laces. Heels are a no, your toes won’t tolerate a heal of any height, toss those to the side. Because your feet are going to swell, and may already be changing shape, also get rid of anything with a narrow toe, pointed toe, or slim instep, you’ll never get them on. How’s the shoe collection looking now? If you’re anything like I was when diagnosed, you’re down to a couple of pairs of clunky slip on shoes. Did I mention you’re attending a wedding this afternoon? Fantastic.
Speaking of weddings, let’s move on to accessories. See that collection of pretty hair ties, barrettes, clips and other things to add a little flair to your hair? In the bin it goes. Don’t worry, the hair will go soon enough, either because it is falling out (a symptom of RA and also a side effect of many RA medications) or because you can’t brush and wash it so you’ll get it cut short and manageable. Speaking of manageable, that jewelry box full of necklaces and bracelets with tiny clasps? Save it for your grand kids, give it to goodwill, you can’t put it on. Same for rings, with fingers that swell when they want to, rings are another great way to get stuck. If you don’t want to have it cut off later, leave it in the box.
At this point, you likely have a massive pile of things you can’t use anymore. Among them, likely some of your favorite things. Frustrated and sad? Welcome to life with RA. That was only what changed in the area of personal care. Notice we never even entered the kitchen or approached any household tasks.
It turns out, life with RA is full of obstacles. Literally every aspect of life is more of a challenge and many things are simply impossible without some sort of adaptive device. The world is full of doorknobs that can’t be turned, bottles and packaging that can’t be opened, stairs that make knees groan, the list is endless, obstacles are everywhere. And chances are…
They hate asking for help
Now that you’ve taken a walk in their clunky slide on shoes, you probably realize there are many times they are going to need help. So many, in fact, that chances are, they are not going to ask every time they need it. If they are stubborn and independent, they won’t ask for help a fraction of the time they need it. They also might not be inclined to let you help. Even on my worst day, I am not interested in help dressing myself. It feels too personal, too much like something a toddler could do, in short, it makes me feel incapable.

They don’t want to feel incapable. They do need help. Offers of help from you, really make their lives easier and make them feel loved and seen. It may be no big deal to you to bend over and pick up those dirty clothes they’ve been staring at all afternoon, to join them in the kitchen and offer to cut the veggies, to offer to help put on that necklace that makes their eyes sparkle. To your loved one with RA, those offers of help are offers of love. They are understanding and empathy. They appreciate them more than you will ever know. It may sometimes be hard to tell because
Pain rules their world and sometimes their attitudes
There is really nothing that alters someone’s sunny attitude like chronic pain. It is hard to be positive when you hurt literally all of the time. When all you want is a break from the constant ache of your inflamed body. It is not at all uncommon for chronic pain sufferers to lash out, become depressed, or both.
On days when pain is more intense, this can become particularly troublesome as your loved one becomes their least lovable self. Try to be patient and understanding. Know that what appears to be anger and frustration with you is actually anger and frustration at their own body. Possibly at themselves, as they beat themselves up for that sugary treat they ate yesterday, the exercise they aren’t getting and all the other little ways they might be contributing to the symptom flare.
Know that what appears to be anger and frustration with you is actually anger and frustration at their own body.
The truth is, it might be something they did, or it might not. Maybe it was that slice of cake that tipped the scale from a daily pain level of 4 to a holy shit, can we just cut my hand off now 9. Maybe it’s the weather, maybe they did too much yesterday, not enough, slept wrong, didn’t sleep. Possible triggers are everywhere, they don’t understand why they hurt, it is incredibly frustrating.
It’s also exhausting. Imagine walking around with the flu all the time. Body aches, exhaustion, brain fog, these are the most frequent and pervasive symptoms of RA. Sleeplessness due to pain and restlessness brought on by medication side effects are also a factor, as the more tired people are, the less tolerant they are of all life’s challenges.

Even good days are full of pain. It is the most persistent symptom your loved one with RA lives with. And no, Aleve doesn’t touch it. Narcotics don’t even touch it most days, not that those are an option for chronic pain sufferers, the dangers of long-term use are too high. They’re left to fight the pain with various over the counter remedies. They learn to live life in pain, to push through days and nights, hoping tomorrow will be better, as they toss and turn on a sea of pain. It is exhausting and undoubtedly increases the other most persistent RA symptom, fatigue.
Fatigue is more than feeling tired
Like chronic pain, chronic fatigue is a bit hard to imagine unless you have experienced it. I used to think it meant you felt tired a lot. I didn’t understand just how exhausted a person could feel until Rheumatoid Arthritis really reared its head. I still find it very challenging to put into words. Imagine you wake up underwater, but able to breath. Every movement feels as though you are dragging yourself through water or better yet, maybe it’s a good thick syrup. You also feel vaguely drugged, like waking up from anesthesia. You’re awake, but definitely not firing on all cylinders. If you’ve ever battled the all-consuming sleeplessness of caring for a sick newborn, imagine that had been 6 babies, and you were all alone, for weeks, that’s fatigue!
Exhaustion, brain fog, memory lapse, an inability to string thoughts into coherent sentences, all aspects of fatigue from RA. It can occur with or without proper sleep. You can sleep 10 hours a day and still feel fatigue. A kind of exhaustion that is unrelated to how much rest you get, there is little your loved one can do but hold on and wait for it to pass. While taking a nap might help a bit, they will undoubtedly wake up as tired as they are when they lay down. It’s a symptom that will go when it is ready and come back when it pleases. It is one of the more frustrating challenges RA brings to the table.
The thing they need most from you is understanding
With a life filled with challenges, fatigue, pain, insomnia, and frustration it is easy to see that what your loved one needs most from you is understanding. They are juggling a rather heavy load, they often have to drop the ball to keep moving ahead, be okay with that. Pick up those dropped balls when you can.
Watch for the things they really struggle with, offer to take them off their plate, or, better yet, surprise them by getting it done while they take a much-needed nap. Encourage them on the hard days. Take time to appreciate the things they accomplish and celebrate the good days with them. Be a sympathetic ear they can turn to when the days are harder. They often feel alone in this disease, be the one they can turn to for understanding.
How Learning to Love Myself Changed Everything

There is a part of my healing story I’ve kept mostly to myself. Sometimes I hint at it, dance around it. I share some of the things I’ve been doing to help myself with the issue, without saying this is why I started practicing these things in the first place. The truth is, one of the biggest hurdles I’ve faced since diagnosis is discovering that I didn’t love myself. The reasons for that are as complicated as falling out of love with someone can be.
The truth is I hadn’t been friends with myself for years. Running from a traumatic childhood through a topsy turvy adulthood, I’d become a master at ignoring my own needs while blaming myself for whatever was going on. Looking back, I now realize I needed therapy, desperately. I needed to acknowledge what I’d been through and let myself off the hook for all that had happened. Running from myself had led to more wrong turns, more regrets, more shame, more blame. I see that now, after a decade of solid work, sifting through that shame and blame, uncovering the roots of my unhealthy relationship with myself.
When I was first diagnosed? I hated myself. I blamed myself for everything that had gone wrong in my life, especially my failing body. I added it to the stack of proof I’d collected over the years that grumbled “you are not enough.” I was sure if I’d worked more, eaten better, taken better care of myself, gone to the doctor sooner, done something different, I would not be where I was. Sick, on the verge of disability, miserably depressed, and mad as hell at myself for all of it.
Feeling like I’d let myself down, I began to try to fix myself from the outside in, asking my body to get stronger, to stop beating itself, while mentally flogging myself with an endless stream of hateful thoughts. Unaware at the time that what we think plays a huge role in how we feel, I made changes in everything from diet and exercise to adding medications. As none of it worked, my disappointment in myself grew. The hateful thoughts came more often.
I still remember the moment when I became aware of the problem. The words that flipped on the switch of awareness and changed everything. “If you wouldn’t let a friend talk to yourself that way, why would you talk to yourself that way?” It blew me away. What a question! Why would I?? I’d shown people the door for treating me like shit in the past. Never would I ever let a friend talk to me the way I spoke to myself. How had it gotten to this point? When did I become my own worst enemy? Most importantly, how could I repair the relationship as divorce was entirely impossible.
Finding out I wasn’t even friends with myself anymore gave me a direction to start poking in. The guidance of my friend and mentor began to place the tools in my hand to start the repair process. Aware of the abuse I’d experienced as a child, Rebecca recommended I start there, do some inner child work, talk to my child self. Try this meditation she said. I’ve rarely cried so hard as I did the first time I did that meditation for healing the inner child. I knew I had to keep going, hard as it would be to face the reasons I had no trust, respect or love for myself, I needed to do it anyway.
I started with some small changes, adding meditation into my routine, breathing exercises, counting myself calm. I practiced grounding and body awareness. I spent time just being uncomfortable in my own skin in the never-quiet of my own mind. Eventually that would shift to comfort and quiet but in the beginning it was loud and painful. With the encouragement of my dear friend, I began to write letters to those who had hurt me and burn them, still my favorite release ritual to this day. I added affirmations to my daily practice, leaving myself little encouragement bombs on post it notes around the house, slowly building a habit of self-love.
Most important of all, I stopped ignoring the mean voice in my head and began redirecting it. I made a deal with myself, for every negative thought I notice, I must stop and tell myself three things I love about myself. At first that was sometimes challenging. It felt silly. I’d roll my eyes at my I love you statements. Or scoff that I didn’t really believe that, as that negative voice fought to stay on board. Eventually I’d make peace with even that part of me and thank it for trying to protect me from myself, adding a forgiveness prayer to my growing self-love toolkit.
It turns out that loving myself requires loving all of me. My strengths and my flaws. The wins and the losses. The good, bad, ugly, beautiful, all of it. Digging in and working on that, shifted so many things. Loving myself led to treating myself with more care. The more I accepted myself, the more love I had for the person I am, the easier the changes I needed to make to feel better became. The things that felt too hard to do without belief in myself, become easier by far with belief on my side. As someone who would do anything to help a loved one in need, one of the best decisions I’ve ever made was to put myself back on that list.
Learning to Lean-How Adaptive Aids Improved My Life

I used to look at adaptive equipment and see it as a flashing neon sign, complete with an arrow pointing at the user (me), “This person is weak” the sign flashed, “can’t do normal things” it sometimes proclaimed. I avoided using tools made to help ease the stress of daily life. After all, those arthritis aids were for people who couldn’t and I could (kinda, with a lot of struggle) but I wasn’t so bad off that I really needed assistive devices, or so I thought. I thought I was fighting to remain independent. It turns out I was just fighting the use of tools that would make tasks simpler for me. Yep, that’s me alright, stubbornly chopping down the trees with a hatchet because I can’t have people seeing me use a chainsaw. The irony? Before diagnosis, I would not hesitate to pick up a tool to make a job simpler. In fact, my creative use of tools was always one of the things I was most proud of, Yankee ingenuity is in my blood. So why the tool avoidance after diagnosis? It turns out, I was more afraid of appearances and the labels they bring than I am stubbornly independent. (Even I was surprised by that one!)

The result of my stubborn tool avoidance? Struggle, giving up, and more tears than this stoic Maine girl is used to shedding. After a few weepy pity parties over the things I couldn’t manage and a complete breakdown involving a water bottle which may still to this day live under the bush I hucked it at, I began to realize I did have a choice. I could continue to struggle or I could get help. Finally starting to come to terms with the limitations RA (Rheumatoid Arthritis) had been putting on my body, I began to consider how I could work around them. That acceptance, that RA was hampering my ability to do, was essential. My first assistive device purchase? A bottle opener, if you have ever lost your shit over an inability to get a drink of water, you know why that was my first toe dip into the world of arthritis tools.
Cut to a few years later and my house is loaded with handy little things that make my life less of a struggle. Bottle openers, dressing sticks, shoehorns, various electric kitchen gadgets, scissors and a whole slew of other helpful aids now live in my home making it safer and more accessible for me, and surprise, giving me more independence. Most of those tools were picked up willingly, some even came with some excitement as I knew they would make me more able. In the fight against disabling disease, that is priceless. Giving myself permission to make that fight easier, shifted things in a small but crucial way.

That is not to say it just shifted all at once and I was able to seamlessly accept all sorts of helpful tools. Quite the opposite. Each set of tools purchased followed an acceptance of their necessity, my need to do. This meant accepting the need for help over and over. If you have followed me long, you may know my stubborn independent nature made that tougher than it probably needed to be. It certainly did when it was time to pick up a cane and eventually a walker.
Some lessons only sink in if we repeat them over and over, accepting help is one of mine. Coming to terms with the fact that my legs were no longer interested in their supportive role, and unable to submit to a life on the couch, eventually led me to accept the need for a cane to help me hobble along. As something I would need outside of the house, making my struggle visible to the outside world, that was not such a simple tool to pick up. In fact, it took extreme need and a moment of desperation for that to happen for the first time. It took a loved one landing in the ICU in critical condition when I had been barely able to walk for a week for me to chose to pick up the cane my doctors had suggested I might find helpful. In the battle between able to get to his side and unable to be there, there was no contest, I had to figure it out, so we stopped and got my first cane on the way.
Since that desperate day, I have made a pact with myself, never let it get that hard before accepting help. Whether that be the assistance of a loved one, or some handy gadget or piece of adaptive equipment, taking help when it is needed, opens life with a disease that often shuts doors to us. It gives us freedom and independence, and perhaps most importantly, it saves our energy for the things we wish to do. Living in a body that can turn the simplest tasks into a struggle, that is a priceless resource.
What handy tools for life with RA can you not do without? I share some of my favorite tools in Handy Arthritis Tools That Reduce The Struggle.
Navigating Winter with Rheumatoid Arthritis

I remember when falling snow brought feelings of wonder and glee. Growing up in the Northeastern US snow and ice were a joy to me as a child. I spent endless hours skating, building snowpeople, sledding and building forts to host icy tea parties and epic snowball fights. Now snow and ice are something I dread. Instead of hoping for a snow day, I spend winter promising myself that someday I will be able to leave in winter, instead of suffering through. There is no doubt about it, the blanket of snow that my younger self adored now brings with it the worst of my RA (Rheumatoid Arthritis) symptoms.
Navigating winter with RA, or any of the other 100+ types of arthritis, is rough. Symptom flares, nasty weather, icy conditions, all increase the challenge of day to day tasks. Over the years, I’ve found a few things that help me keep moving when the world freezes over.
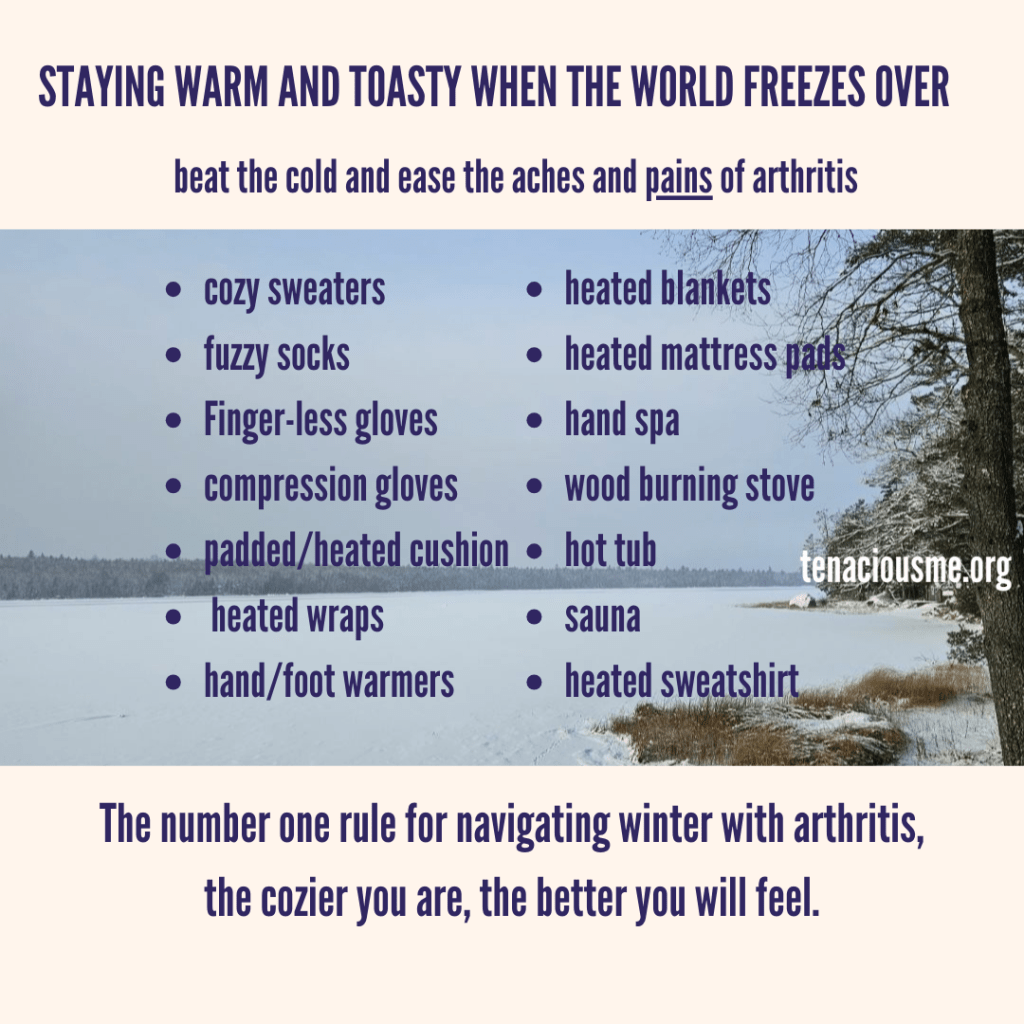
The first and probably most obvious is staying warm. If you have any type of arthritis you know what it feels like when you get too cold. With RA that bone chilled stiffness and pain can invade my entire body. I’ve developed a deep love of cozy sweaters, fuzzy socks, and all things snuggley and warm. Finger-less gloves help keep my hands toasty, whether I’m inside or out. A pair of light compression gloves like my favorites from Grace and Able, are perfect for a little extra warmth when inside. When I do get chilled, I use heated blankets, heating pads, and anything else that will warm me up to chase the cold (and pain) away.
My second big winter challenge is ice. Every winter 1 million Americans are injured in a winter slip/fall accident. In fact, most of the slip and fall injuries occur at this time of year. With an artificial hip and a few mobility challenges, I have learned to be extra careful in icy conditions so that I remain upright! From choosing footwear with good tread to strapping on ice cleats and using a walking stick with an ice tip, the strategies I use vary depending on the amount of ice I’m going to need to navigate. One of my consistent strategies no matter how much ice, walk like a penguin. No, I’m not kidding, those tuxedo-ed flightless birds certainly have perfected the art of the slow and steady waddle. It might take longer to get where I am going, but the time saved healing broken bones is well worth it.
Another challenge winter brings is an increase in the spread of cold and flu. Because my immune system is knocked down to keep my disease managed, I have to be extra careful to avoid germs this time of year. Making sure to wash my hands, excusing myself when someone in the group appears to be unwell, and making sure I am well nourished all help support my health this time of year. Choosing to wear a mask in situations where I wont be able to keep my distance also helps protect me. Making sure I am eating well and taking vitamins, including vitamin D, helps me fend off the germs I couldn’t avoid. Eating well also helps reduce my inflammation and keeps me moving.
Staying mobile is another challenge that becomes more of a struggle when winter settles in. Snow and ice limit my options for taking a walk, my favorite intentional exercise. Gardening is also not possible under a layer of ice. Though I’ve never been a big fan of indoor exercise routines, they are a necessary part of my winter survival plan. Making sure I stay active and strong supports my joints and keeps me mobile. Building movement and stretch breaks into my daily routine helps ensure that this less active time of year doesn’t set me back.
While there are certainly plenty of challenges to consider, there are a few things winter is actually great for. Leaning into the slower pace of life, it is a great time for rest and recovery. Starting each day with some journaling and diving into a self help program of some sort are part of my personal winter routine. Filling my days with good books, learning new things, and crafting also helps me pass the time without going stir crazy. Taking time to plan summer getaways and sketching out a plan for the coming growing season also prevents the cabin fever from settling in and keeps me looking forward to warmer days.

With a little extra self-care, a bit of caution, and all the warm things you can get your chilly little paws on, winter doesn’t have to be the season of endless suffering. You might even find some pretty great days, between storms of course. They’ve yet to make a cure for those weather related symptoms every arthritis sufferer lives with. Until they do, I’ll be spending these stormy days snuggled up with my electric blanket and a big steamy cup of chai green tea, plotting my escape to warmer destinations.
What gets you through winter with rheumatoid arthritis?

My Tiny Craft Obsession

If you follow me on social media, you may have noticed I’ve got a small hobby I share from time to time. Creative by nature, I have enjoyed crafting for as long as I can remember. Some of my earliest memories are sewing lessons with my mom and the endless hours I spent making finger crochet chains, though I can’t recall who taught me to create those. As I got older, I dabbled in many different types of crafting, from fiber arts like weaving and macrame to beaded jewelry and wire wrapping. After being diagnosed with rheumatoid arthritis, I set that aside for quite some time. After all, when you barely have time and energy to keep up with taking care of yourself, let alone your family, sitting down to create something feels like a selfish waste of time. Besides, most of my craft hobbies had become challenging, and I was blaming them for helping me ruin my hands at the time. All that beading, crocheting, loom knitting, hand sewing…couldn’t have been good for me, right? Well…it turns out, yes but no.
The fact is, there are some crafts I probably cannot do. Things that require a large amount of hand strength are always going to be hard because I just don’t have very strong hands. Spending big chunks of time hunched over a project will always do me more harm than good because I can’t sit and do something for long chunks of time, especially not something that puts me in a challenging posture. Giving away all of my crochet hooks and yarn though, a bit of an overreaction. I would come to find that I can and should crochet. For short chunks of time, with frequent stretch breaks. Using chunky handled crochet hooks, I began making my own fingerless gloves and washable cane handle covers.
Slowly, I started considering the other things I might do. By now officially disabled, years into walking this new path, I’d learned a lot about managing my disease. The importance of living a full life no matter what that looks like. How vital it is to seek those sparks of joy; the world becomes terribly dark without them. Creating lights me up. It gives my brain and body an outlet. Done right, I’ve found it wonderfully therapeutic, both mentally and physically. The key for me has been mostly in pacing. In taking small bites out of a project instead of finishing it in one day. It is no surprise that I’ve found my niche in crafts with built in pacing, resin art and miniatures. The resin must cure. The paint or glue has to dry. Most steps are quickly done and then, there is some waiting. Perfect time for a stretch break. Excellent window for a quick chore and some bigger body movement while I wait to do the next coat of paint.
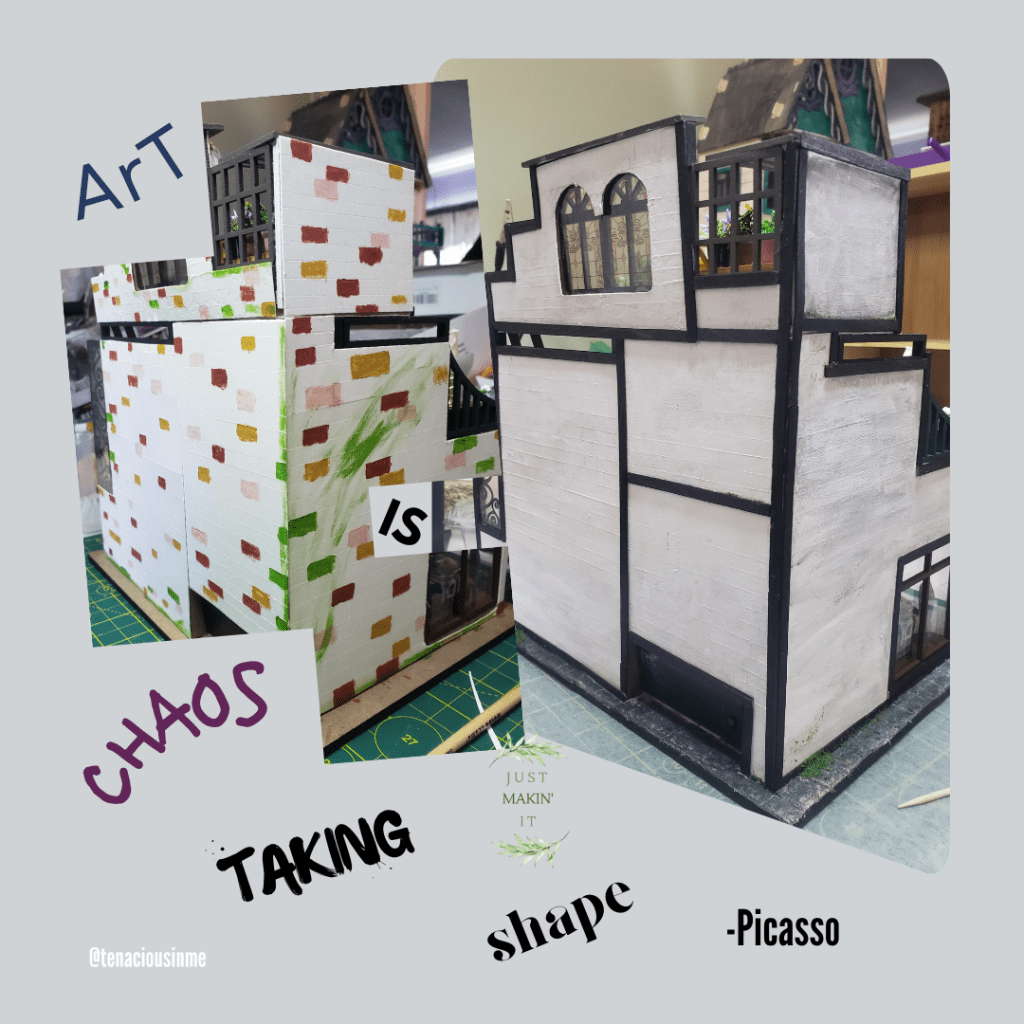
It turns out, creating tiny worlds is something I’m very capable of. I can turn a pile of trash into something really surprising. Applying my love of design and construction on such a small scale makes it doable for me. Building a cabinet may be too much for me to tackle, building a 2-inch-tall cabinet isn’t. These miniature creations also allow me to use a wide variety of skills and art mediums. The variety not only keeps me entertained, but it also makes it easier for me to accomplish as I’m not spending long chunks of time doing any one thing. Sculpting, painting, cutting, fabric arts, having a wide variety of things to do means I can switch between them and avoid repetitive stress, something my body has no tolerance for.





Spending precious resources, time and energy, on something that I enjoy no longer feels selfish. It feels therapeutic. Crafting challenges my dexterity and helps me maintain both strength and mobility. Creating allows me to escape, to sink into a world of imagination, to breathe life into something I see in my mind.
Have a hobby that helps you escape or makes your life with a chronic illness more bearable? Tell us about it in the comments, we’d love to hear your story!
Want to support my tiny craft obsession? Check out my Etsy shop, Just Makin It In Maine, for some cute handmade crafts.
Gardening with RA 2024

If it seems like my yearly gardening post is a bit late this season, well, that’s because it is! Those who follow my blog know, gardening is one of my favorite types of therapy, both physical and mental. Spending time helping things grow, relaxes me. Having living things dependent on me showing up to nurture them , motivates me to move a little more, even on a rough day. The tricks I’ve learned over the years, help keep that workload manageable. Gardening after all, can be back breaking, hot work. A few changes to the way I approach the task make it a (mostly) painless process.
Raise it up- I do very little of my growing at ground level. That is, in fact the true story of why this post is so late! I wanted to show you what we’ve been up to this spring/summer. As the first growing season since we settled into our own home we’ve had a lot on our plates this spring. Reclaiming and cleaning up our jungle of a yard and beginning to establish my first stationary raised beds has taken time, energy and the hard work of my luckily very willing boys. Raising the level of the growing things I need to tend means less stooping and bending to pull the inevitable weeds, prune plants and harvest. Before raised beds, I gardened in fabric bags and raised pots on platforms.
Weed prevention- Preventing weeds from growing is by far my favorite type of weed management. Putting down a good weed barrier is the first line of defense. Lining your raised bed with cardboard or a commercial weed barrier will help prevent weeds from growing up through the ground and invading your beds. A good heavy mulch can also help keep weeds at bay, as well as helping slow water loss to evaporation. This means less weeding and less watering! I use a variety of mulches from wood chips to shredded paper and newspaper.

Simplify watering- One of the tasks that can be a huge pain without the right setup, is watering. Dragging heavy hoses or watering cans around wears me out quickly. Investing in a few lightweight expanding hoses, using lever activated spray nozzles instead of trigger style ones, and raising shutoffs for easy access all make the task much simpler. When I do use a watering can, I use a small one with a large easy grip handle that I can pour with two hands. Next year, we will start adding in-ground irrigation, which will make watering as simple as flipping a switch or setting a timer.
Get the right tools for the job– Gardening with arthritic hands and knees comes with it’s challenges. Most of them can be overcome with the right tools. Long handled tools mean less stooping, chunky handled tools improve my grip and are easier to work with. Electric trimmers make pruning tasks more manageable. Weeding robots are on the market though sadly not yet in my own garden. For now, weeding tools with long chunky handles will have to do. Raised gardens make things easier on my knees and back, my travel stool also spends a lot of time in the garden as switching between standing and sitting keeps my body happier.

Pacing- While there is a part of me that wants to jump right in and have acres of gardens, there is a much more realistic side that knows that will set me and the plants up for failure. Starting with a couple of small raised beds and some patio pots, adding perennials slowly, keeps the work load small enough so everything is getting what it needs. Breaking tasks like planting, thinning, and weeding into several short sessions instead of trying to do the entire garden at once, means I actually get them done. Rather than spending 3 days recovering from pushing myself too far, I spend a little bit of 2-3 days doing the weeding. A little bit at a time, it all gets done.
Ask for help- Some garden tasks are heavy, some are just too much of a struggle, or will definitely make part of my body really angry. Those are the things I am most likely to ask for help with. Building raised beds by myself, is not something I would tackle. Luckily, I’ve got some pretty great help. Together we are creating the gardens of my dreams, one little step at a time.
Do you enjoy growing plants? What is your favorite RA friendly garden tool?
Let’s Talk About Disability

Some words seem to hold more power than others. Joy, sorrow, mother, father, these words likely create an instant picture or sensation when you read or hear them. Exactly what that picture looks like, depends on the experiences you’ve had with them in your lifetime. Disability is one such powerful word, the shape and power of which is created by our relationship to it.
Before becoming disabled myself, had I been asked I would have told you that disabilities are usually obvious, always challenging, and hard to live with. My experience with disability was that of distance, I’d never really gotten up close and personal with it. I hadn’t sat with it day after day. I didn’t have personal experience with it. It hadn’t occurred to me how many forms it could take, how it may or may not shape a life. I was clueless to the existence of invisible disabilities. If the term “dynamic disability” had been coined, I’d certainly never heard it.
Years into being deemed disabled, my understanding of the word has both deepened and shifted. I’ve come to understand both static disability (permanent disabling physical changes) and dynamic disability (disabling physical symptoms that come and go) on a very personal level. The physical limits my body has do have a very real impact on my way of life. There are things I just cannot do without some kind of assistance. There are things I should not do because then I won’t be able to do anything the next day. Some days I need a lot of help with everyday tasks. Other days I can get by with the help of a few handy adaptive aids.

Yet, even with all this personal experience, I admit, I still struggle to label myself disabled. Somewhere along the way, that word took on a bigger, darker meaning that I cannot seem to shake. It imposes limits, sets boundaries. Disabled suggests I cannot. Can I open a heavy door alone? Not easily, no. If I were to put my mind to it could I figure out a way to get it open? My ability to escape most public bathrooms says yes, indeed I can and have figured out how to lever those heavy security doors open when necessary.
In fact, there are tools and workarounds for just about anything a person needs to do. Which makes it much less about what I can and can’t do and more a question of how much of a challenge it will be for me to do it. As my experience with disability deepens I see it both more and less clearly. No longer is it so very cut and dry. The line between able and unable, it turns out is blurry and depends on so much more than physical ability or lack thereof.
Perhaps that is why the label is one that I struggle with. Nothing about it is simple, not even defining it. It’s no wonder I struggle with using it to define my own existence.
When you think about the word, disabled, what does that look like to you? What feelings does it bring up?